DDMFR Part A - Sample questions - radiological sciences and techniques module
Question 1: What practical steps are taken to reduce patient risk during intraoral radiology?
Similarly, to other areas of radiology, the Ionising Radiation (Medical Exposures) Regulations 2017 (IRMER17) apply to dental radiology. The regulation is designed to protect patients and staff from harm arising from radiation where possible. They state that medical exposures must be optimised and justified.
As well as duties for the employer, IRMER17 sets out duties for the referrer, practitioner, and operator with respect to patient safety. Staff must have appropriate on-going training and competency assessment to ensure the most up to date techniques are used to optimise patient
dose. The referrer must provide all the relevant clinical information for the practitioner to decide on whether the exposure is justified. Only justified examinations are carried out.
The operator is responsible for carrying out the exposure using the correct set up as well as checking to ensure repeat images are avoided.
The equipment used must be optimised to ensure that the patient dose is as low as reasonably practicable (ALARP) whilst proving a diagnostic quality image. The equipment should be high kV (60-70kV), ideally using a constant potential and have a long focus –to skin distance. Rectangular collimation should be used in conjunction with image receptor holders. A digital imaging receptor/ F-speed film should be used.
The equipment is checked through a quality assurance programme set out by the MPE. New equipment must also be checked by the medical physics team before its first use and accepted
into clinical used by an MPE. There must also be a risk assessment in place for areas where radiation is used. Imaging protocols will have different exposure factors (kV, mAs) depending on the type of examination and whether the patient is an adult or child.
PPE is not recommended for patients in dental radiography. It is likely that shielding organs such as the salivary glands or brain will obscure the radiation beam. Eyes should be outside of the primary beam. Although a thyroid shield can be useful in some examinations, it has been shown that the exposure factors, technique, and collimation can be more effective at reducing thyroid dose. Dose to other organs is likely to be caused by internally scattered radiation and therefore
PPE wouldn’t be effective.
Pregnancy should not exclude patients from having dental radiography, but using modern techniques, the abdomen should not be in the primary beam and PPE is not required.
Overall patient safety in dental radiography is managed through risk assessments, training, dose optimisation and well-maintained equipment. Where there have been accidental or unintended exposures the incident must be reported and investigated.
Question 2: Describe the Compton effect and how it is relevant to dental radiology
Contrast in diagnostic images using x-rays results from the different attenuation of photons by the different tissues in the body. Photons interact with matter through the photoelectric effect,
Compton effect and pair production to a degree that varies with tissue and photon energy. In dental radiology the tissue interactions are dominated by the Compton effect. This is because Compton scattering dominates at the photon energies commonly found in dental radiology and also because the electron density of the tissue means that the probability of a photon interacting with an outer shell electron is high. The Compton effect is independent of Z.
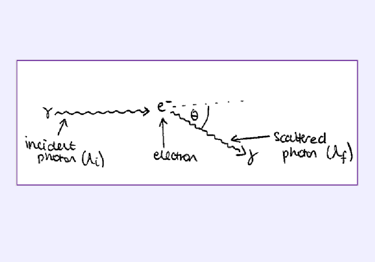
The Compton effect occurs when an incident photon interacts with an outer shell electron. The photon is scattered by the electron and the electron is excited by the photon. The energy of the photon after the interaction is dependent on the angle of scatter. The change in wavelength of the electron, ∆𝜆𝜆, can be calculated using Planck’s constant, ℎ, the mass of an electron, 𝑚𝑚, and the speed of light, 𝑐,
∆𝜆𝜆 = ℎ/𝑚𝑚𝑐𝑐 (1 − cos(𝜃𝜃)).
A diagram of the Compton effect is shown below. In dental radiography, a large proportion of the scattered photons exit the patients head and are not absorbed by the patient. These photons
can contribute to the radiation dose of staff and the public which is why it is important to use the principles of radiation protection (time, distance and shielding).
The Compton attenuation coefficient (the likelihood of a photon interacting with tissue via the Compton effect is proportional to the electron density of the tissue, the mass density of the tissue and inversely proportional to the energy of the incident photon. The Compton effect will attenuate more photons in materials with a high electron density and high mass density, providing contrast in the image. In dental radiology the area being imaged usually consists of
soft tissue, bone and amalgam. Of these materials amalgam has the highest mass density and the highest electron density therefore the Compton effect attenuates more photons in the amalgam. Soft tissue has the lowest mass density and electron density therefore the Compton effect is less prominent, fewer photons are attenuated.
As a general principle, scatter contributes to dose of the patient and staff member and limits image quality.
Question 3: Describe what happens during processing of a photostimulable phosphor plate (PSP) used in dentistry?
Imaging plates can be used for both intra oral and extra oral radiography.
After exposure, PSPs should be processed as soon as possible because trapped electrons spontaneously release over time.
Phosphor plates absorb and store energy from x-ray radiation and release this energy as light (phosphorescence) when stimulated by another light of an appropriate wavelength.
The PSP material used for radiographic imaging is “europium-doped” barium fluorohalide on a flexible plastic backing support.
When exposed to a radiation, valence electrons in europium absorb energy and move into the conduction band. These electrons migrate to nearby halogen vacancies in the fluorohalide lattice and may become trapped there in a metastable state. The number of trapped electrons is proportional to x-ray exposure and represents a latent image.
When stimulated by red light of around 600 nm, the barium fluorohalide releases trapped electrons to the conduction band. When an electron returns to the EU+3 ion, energy is released as light in the green spectrum.
Fibreoptics conduct the light from the PSP plate to a photomultiplier tube. The photomultiplier tube converts the light into electrical energy. A red filter at the photomultiplier tube selectively removes the stimulating laser light and the remaining green light is detected and converted to a varying voltage. The voltage signal is quantified by an analogue to digital convertor and stored and displayed as a digital image.
PSP plates must be erased to eliminate residual images from previous exposures. This erasure is accomplished by flooding the plate with bright light. Current PSP scanner systems integrate automatic plate erasing within the scanner.
Erased plates are placed in light tight containers before exposure.
Question 4: Paul is a 19-year-old who has fallen from his bike and sustained a fractured mandible and complicated fractures of his upper central incisor teeth. Clinically he has no other injuries.
A panoramic radiograph shows a guardsman fracture. He requires a posteroanterior of the jaws (PA jaws/mandible) and an upper standard occlusal view. Describe the operator radiographic technique for each examination from after patient identification to pressing the exposure button.
Upper standard Occlusal radiograph (50% of the allocated marks)
- The patient is seated upright with the head supported and with the occlusal plane horizontal and parallel to the floor.
- A dental X-ray set is used. Exposure factors set
- Rectangular collimation used. However round collimation may be used if there is doubt that the area of interest will not be fully covered.
- A thyroid collar / thyroid protective shield positioned.
- The size 4 image receptor is placed flat in the mouth on the occlusal surfaces of the lower teeth and the patient is asked to gently bite together to avoid receptor damage.
- The image receptor in this adult patient should be placed centrally with is long axis crossways.
- The dental x-ray tube-head is positioned in the midline aiming down through the nasal bridge at an angle of 65-70 degrees to the image receptor.
Diagrams may be used to illustrate the above answer.
PA (Posteroanterior Mandible (PA mandible) (50% of the allocated marks)
- A skull unit or Bucky is used with the image receptor vertically positioned.
- Exposure factors set.
- Appropriate collimation applied to ensure entire mandible included.
- The patient’s head is positioned facing the image receptor. The head is tipped forward so that the forehead and nasal tip are in contact the image receptor i.e. the forehead – nose position, so that the radiographic baseline (orbitomeatal baseline) is horizontal.
- Median sagittal plane of the patient is perpendicular to the image receptor.
- The x-ray tube head is horizontal and perpendicular to the image receptor with the central ray centred through the cervical spine at the level of the mandibular rami / angles.
Diagrams may be used to illustrate the above answer.